Learn about Dysautonomia from Brit Adler, MD, Assistant Professor of Medicine, Division of Rheumatology, Johns Hopkins University School of Medicine.
Dr. Adler is a translational physician-scientist with an interest in postural orthostatic tachycardia syndrome (POTS) and dysautonomia that can occur in COVID and Lyme disease patients. She evaluates patients in the Johns Hopkins Autonomic Testing Lab and performs the tilt table test and other evaluations.
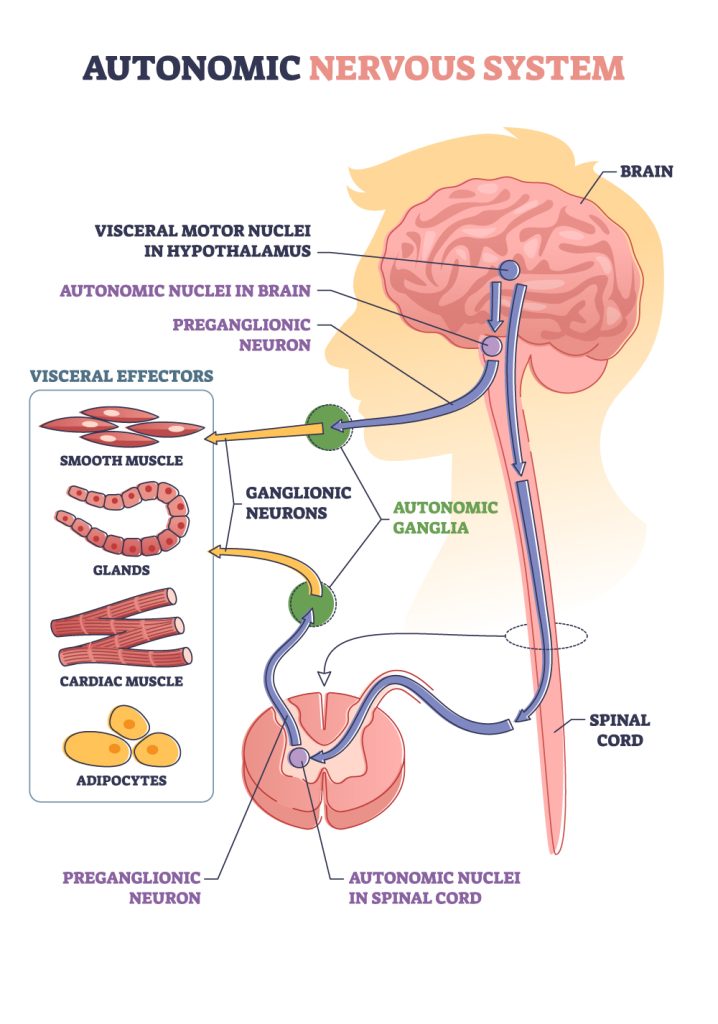
What is Dysautonomia?
Dysautonomia is dysfunction of the autonomic nervous system.
The Autonomic Nervous System regulates:
- Heart rate and blood pressure
- Gut motility
- Body temperature
- Sweating
- Tear production
What is POTS?
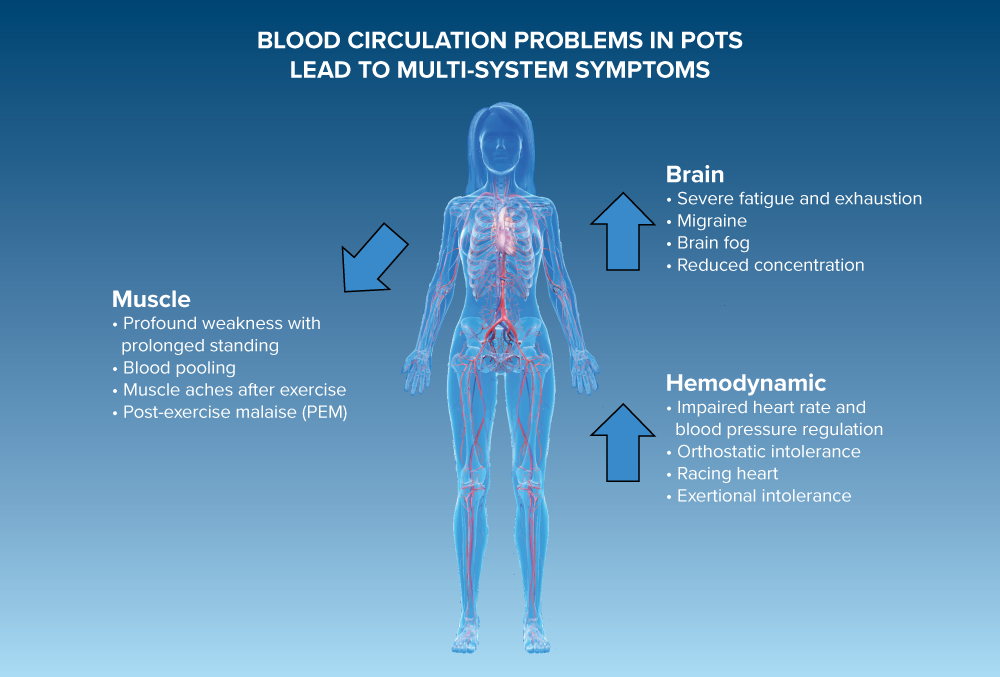
A common manifestation of dysautonomia is POTS or postural orthostatic tachycardia syndrome.
POTS is the result of impaired heart rate and blood pressure regulation that results in orthostatic intolerance. Orthostatic intolerance is the clinical manifestation of brain fog, fatigue, dizziness, and weakness made worse by prolonged standing.
Symptoms can be debilitating and include:
- Brain fog
- Severe fatigue and exhaustion
- Profound weakness with prolonged standing
- Racing heart
- Exertional intolerance
- Muscle aches
- Dizziness
Can Lyme Disease cause POTS?
Yes, individuals may get dysautonomia and POTS following a Lyme disease infection.
What testing is available to clinicians to diagnose dysautonomia?
Tests for POTS
- 10 Minute Stand Test
- Done in a doctor’s office to measure blood pressure and heart rate while standing for 10 minutes
- Heart rate increase of more than 30 beats per minutes with standing is diagnostic of POTS
- Tilt table test
- A more complicated test that includes continuous monitoring of heart rate and blood pressure while lying down and while suspended in an upright position on a tilt table
Tests for other aspects of Dysautonomia
- Motility testing for gastrointestinal dysautonomia
- Determines what area of the gut is affected
- Quantitative sudomotor axon reflex test (QSART)
- Measures the nerves that control sweating
- Skin biopsy to detect small fiber neuropathy, which is commonly present in patients with dysautonomia
- Detects decrease in density of the small nerve fibers in the skin
In the future, the Johns Hopkins Autonomic Testing Lab is planning to also offer:
- Transcranial Doppler Ultrasound
- Measures the change in blood flow to the brain with tilt
What are the limitations of current diagnostics?
Dysautonomia is a dynamic disease that can wax and wane, and diagnostic tests on a patient’s good day may not have positive findings despite the patient’s history of symptom flares.
Potential Risk Factors for POTS
- Genetic and autoimmune susceptibility
- POTS disproportionately affects young women
- Hypermobility or Ehlers Danlos Syndrome (EDS)
Treatments for Dysautonomia
Beneficial lifestyle approaches
- Increased fluid and salt intake to optimize circulation and improve blood flow
- Compression stockings
- Abdominal binder to help pump blood back up to the heart and brain
- Patient-tailored exercise programs designed for patients with dysautonomia since exercise may not be well-tolerated
Medications
- Medications to improve gut motility
- Medications to improve circulation
- By reducing heart rate
- By increasing blood pressure
- Medications to target autonomic nervous system
- In clinical trials, immunomodulating medications such as IVIg (Intravenous Immunoglobulin) are being studied
- Antimicrobials for ongoing infections
Many infections are associated with POTS. Different infection-associated POTS syndromes present with similar symptoms and may share common underlying mechanisms.
POTENTIAL MECHANISMS UNDERLYING INFECTION-ASSOCIATED DYSAUTONOMIA
The autonomic nerves or autonomic ganglia may be affected by:
- Chronic infection
- Autoimmune response triggered by an infection
- Damage to autonomic nerves by an infection
- Neuro-inflammation triggered by debris left-over after an acute infection is treated
CHRONIC ILLNESSES ASSOCIATED WITH POTS
- Post Treatment Lyme Disease
- Long COVID
- Myalgic Encephalomyelitis/Chronic Fatigue Syndrome or ME/CFS
- Sjogren’s Syndrome
- Systemic Lupus Erythematosus
- Hashimoto’s Thyroiditis
- Celiac Disease
- Diabetes
- MS
- Other Infection Associated Illnesses


